Radial Artery
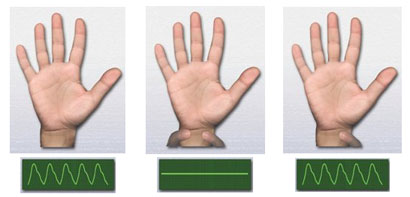
First, the arm that Radial Artery graft will be prepared to be checked for whether it is fed from Ulnar Artery or not. Modified Allen test (R. Wolf) is used for this. Pulse oximetry is attached to one from first three fingers and both Ulnar and Radial arteries are suppressed until the pulse tracing to draw a straight line. If the tracing returns to its previous shape when ulner artery left, this mean that ulnar artery will be sufficient to feed the hand.
The patient is begun to be administered diltiazem infusion at a dose of 1 µg/kg/hour with the anesthesia induction. Complete of the arm from which the artery will be excised is prepared according to surgical principles and covered. Radial artery is begun to be excised during the preparation of internal mammary artery.
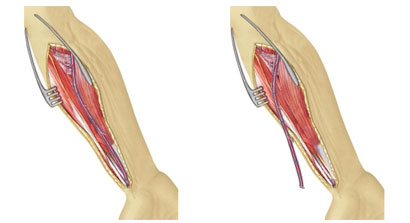
Beginning point of the skin incision is the lower tip of Antecubital Fossa at proximal at which brachioradial muscle and Biceps tendon connect. Then it goes on from this point in accord with the curve of brachioradial muscle and progresses at distal between Flexor Carpi Radialis tendon and Radial bone ridge, and it is ended at 1 cm to the wrist. Subcutaneous incision is also done in accord with the skin incision and while Radial Arter is observed in the artery-nerve capsule at distal, the incision goes on under the brachioradial muscle group at proximal. Flexor Carpi Radialis Fascia and Brachioradial Fascias splits apart as Lateral Antebrachial Nerve (LAN) that provides skin innervation of the forearm, left at the lateral. In this way, the nerve in the fascia will stay away from the surgery site during dissection. When an ecarteur that will split apart the two muscle is inserted, complete of the Radial artery will be revealed. Superficial Radial Nerve (SRN) innerves the first three fingers of the hand, and it is neighbor to Radial Arter at the third distal part.
Radial Artery, is most easily dissected at the mid third part. After it is released from top and bottom, dissection is continued first to distal and then to proximal. Radial Artery is never held, adherent veins can be held and pulled slightly if necessary. While side branches are thinner, shorter and more frequent at distal (care must be taken during dissection), they are thicker and more rare at proximal. Protection of the SRN at distal and LAN at proximal is important in terms of sensation defects. Radial artery is dissected up to Superficial Palmar Artery at distal and Radial Recurrent Artery at proximal. Bleeding control is performed after the artery completely releases.
The distal of Radial Artery is ligatured with 3/0 silk as to Superfacial Palmar Artery will be protected. The artery is cut from proximal of ligation and provided to bleed up to 50 cc in a container, including 5 mg verapamil, 5000 iu heparin, 5 mg nitroglycerin and 10 cc isotonic serum (Florence Nightingale Solution). Then distal of the artery is closed with a clip. Similar to distal incision, a proximal incision is also performed as to Radial Recurrent Artery will be protected. After Radial Artery is dissected, verapamil is injected in it with a Teflon catheter, and it is protected at 30oC in a previously prepared liquid until it is used. Proximal and distal stumps can be supported with transfixion sutures or clips. Fascias that were opened in the forearm can be approached to each other one by one with sutures. Subcutaneous is closed with 3/0 polyglactin, and skin is intracutaneously closed with 4/0.